Laparoscopic Gastric Banding
What is gastric banding?
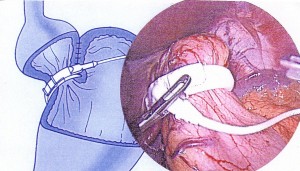
Gastric banding is purely restrictive procedure. It involves applying a band around the top of the stomach forming two portions of the stomach – a proximal small ‘pouch’ of about 15cc and a distal large normal stomach. The band is connected via a narrow tube to a reservoir ‘port’, which is kept underneath the skin usually over the breast bone or below or over the lower ribs. The band could be adjusted by removing or injecting fluid into the ‘port’. This restricts the food that can pass through the stomach. Even a small amount of food will stretch the ‘pouch’ and create the feeling of fullness. It has the advantage of being relatively safe, less complex & reversible, but requires close follow-up to decrease the size of the stomach pouch outlet as the band is inflated over a period of weeks. That’s why failure rate is high. Diabetes and hypertension may be resolved (less than 50%) once the weight loss is achieved.
How long will it take to recover after surgery?
As the surgery is performed laparoscopically, patients typically spend less than 24 hours in the hospital . It takes most patients about 2 weeks to return to work (some go to work within a week) and a month to resume vigorous exercising. In the case of open surgery or if there are complications, recovery may take longer.
What are the Risks from Gastric Banding?
Operative risks of injury to the viscera and bleeding are rare. Infection of the port can happen (1:100) which may have to be removed leaving the band in situ. Nausea and vomiting, gastroesophageal reflux (regurgitation), band slippage/pouch dilatation and stoma obstruction (stomach-band outlet blockage) are the most common late band complications.
What are the late Gastric Banding Complications:
• The band can spontaneously deflate because of leakage. That leakage can come from the band, the reservoir, or the tubing. This requires operation to replace the band if the band is leaking, replace the port if the port is leaking or to trim the tubing if the tubing is leaking.
• The band can slip. Stomach may come through it. The stomach pouch can enlarge. The pouch could become gangrenous and perforate resulting in peritonitis. Band may have to be removed, repositioned or removed and converted to bypass/sleeve gastrectomy/DS
• Ulceration: The band can erode into the stomach: Remove Band. Any further procedure – Sleeve gastrectomy or gastric bypasscan be performed after at least 3 months
• Gastritis (irritation of stomach). May need antacids/PPIs
• Heartburn/ gastroesophageal reflux (regurgitation): Deflate the band. If it doesn’t work, remove the band
• Dysphagia (difficulty in swallowing). Band may have to be deflated.
• Dehydration due to vomiting. Band may have to be deflated
• Constipation due to the altered food and low fluid intake.
• Band Failure or Weight regain due to going back to old habits or becoming sweet eater or band is loose : require further procedure – Sleeve Gastrectomy or gastric bypass. Access port may be leaking or twisted: require another procedure to correct it.
• Nutritional deficiencies if not taking a balanced diet.
Obstruction of the stomach can be caused by ofod, Swelling, Band erosion, the band being over-inflated, Band or stomach slippage / Stomach pouch enlargement, Stomach pouch twisting. Tightening the band too fast or too much to try to speed up weight loss should be avoided. The stomach pouch and/or oesophagus can become enlarged as a result; it may cause erosion of the stomach. You need to learn how to use your band as a tool that can help you reduce the amount you eat. Some patients have more nausea and vomiting than others. You should see your physician at once if vomiting persists; the band has to be deflated immediately or even removed.
Is there a chance the band will need to be removed?
The GASTRIC BAND is a long-term implant, but it may have to be removed or replaced at any time. For instance, the device may need to be removed to manage any adverse reactions you might have. The device may also need to be removed, repositioned or replaced if you aren’t losing as much weight as you and your doctor feel you should be losing.
Will I feel hungry with the Lap band?
The gastric band makes you eat less and feel full in two ways – first by reducing the capacity of your stomach and second by increasing the time it takes food to get through at the stomach. After a small meal, you should feel full. If you follow the nutrition guidelines when you choose your food and then chew it well, you should not feel hungry or deprived. Remember that the Lap band is a tool to help you change your eating habits.
Will I vomit a lot after the operation?
The gastric band limits food intake. If you feel nauseated or sick on a regular basis, it may mean that you are not chewing your food well enough or that you are not following the diet rules properly. Contact your doctor if this problem persists. Vomiting should be avoided as much as possible as it can cause the small stomach pouch to stretch. It can also lead to slippage of part of the stomach through the band or cause erosion of the band into the stomach. In such circumstances you may have to have the band removed.
How much weight will I lose?
Weight-loss results vary from patient to patient, and the amount of weight you lose depends on several things. The band needs to be tight enough to restrict your food and you need to be committed to your new lifestyle and eating habits. Obesity surgery is not a miracle cure, and the pounds won’t come off by themselves. It is very important to set achievable weight-loss goals from the beginning. You lose a lot of weight initially. Twelve to eighteen months after the operation, weekly weight loss is usually less. The main goal is to have weight loss that prevents, improves, or resolves health problems connected with severe obesity.
How frequently have I to visit the doctor after surgery?
Regular Check-ups are necessary. Patients are seen 2 weeks after the surgery and then every 2 – 12 weeks for the first year. Adjustments are performed during some of these visits. It is typical for follow-up visits to be scheduled every three to six months during the second and third year, depending on the individual case.
Does the Lap band limit any physical activity?
The gastric band does not hamper physical activity including aerobics and strenuous exercise.
How is the band adjusted?
Adjustments are often done in an outpatient clinic under local anaesthestic. Sometimes Adjustments may be carried out in the X-ray department. A fine needle is passed through the skin into the access port to add (‘fill) or subtract saline; this will tighten or loosen the band.
Can the band be removed?
It can be, usually laparoscopically. The stomach generally returns to its original shape once the band is removed. After the removal, though, you may soon go back up to your original weight. You may also gain more weight.
What will happen if I start vomiting?
One of the major advantages of the gastric band is that it can be adjusted. The band can be loosened by removing saline from it. When you have recovered from your illness and want to lose weight again, the band can be tightened by increasing the amount of saline. If the band cannot be loosened enough, it may have to be removed or unlocked by surgery.
What about pregnancy?
Wait for at least 18 months when your weight becomes stabilized. Becoming pregnant can be easier as you lose weight. Your menstrual cycle may become more regular. If you need to eat more while you are pregnant, the band can be loosened. After pregnancy, the band may be made tighter again and you can resume losing weight.
Will I need to take vitamin supplements?
You may. It’s possible to not get enough vitamins from three small meals a day. At your regular check-ups, your specialist will evaluate whether you are getting enough vitamin B12, folic acid, Vitamin D and iron. Your surgeon may advise you to take supplements.
What about other medication?
Break big tablets into small pieces or dissolve them in water so they do not get stuck in the stoma and make you sick. You may have to take H2 blockers like Ranitidine or Proton pump inhibitors like Omeprazole, Lansoprazole if you are taking aspirin and other non-steroidal anti-inflammatory pain relievers (Ibuprofen, Diclofenac) because they may irritate the stomach. The ulcer/erosion these drugs may cause could result in band removal.
What about alcohol?
Avoid excess alcohol intake. Alcohol has a high number of calories.
What can I eat?
You may eat most foods that don’t cause you discomfort. However, because you can only eat a little it is important to include foods full of important vitamins and nutrients. If you eat foods that contain lots of sugar and fat or drink liquids full of “empty” calories, such as milkshakes, the effect of the band may be greatly reduced.
Warning! : Contains live recorded footage of Weight loss surgeries. May not be suitable for all viewers.